Download the PDF version: Seven Qualities To Seek In A Service Provider
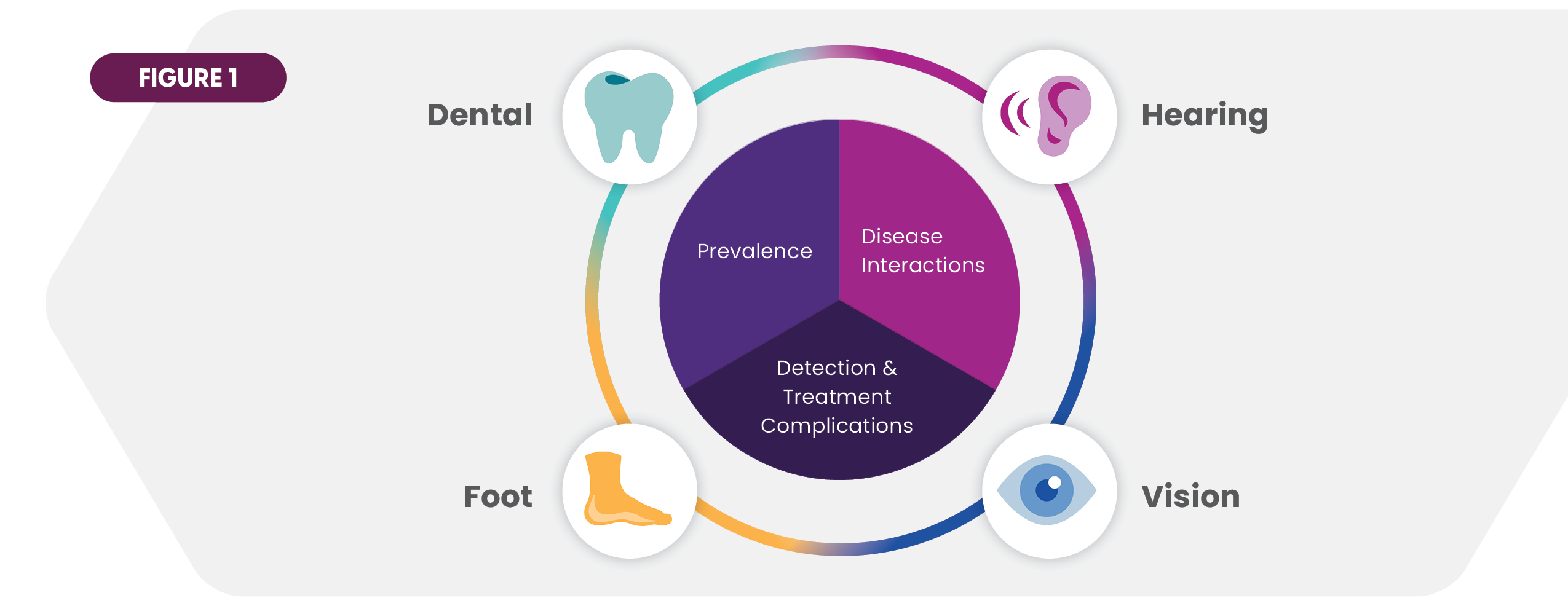
Delivering effective care in today’s skilled nursing facility (SNF) is a complex undertaking. Residents frequently have multiple health issues, and many possess risk factors for illnesses or conditions that may develop during their stay. Dental, vision, hearing and foot/lower leg medical problems are particularly prominent and merit a high degree of attention. This article takes a multifaceted look at the challenges facing SNFs in providing quality care in these four medical specialties. A proven solution of engaging an onsite care partner is also explored, highlighting seven qualities to seek in a services provider.
Charting the Complexity of Care
Dental, vision, hearing, and foot conditions occupy an important place in the SNF care portfolio. They are simultaneously prevalent among residents, pose frequent barriers to care, and prone to interact with other serious diseases and illnesses.
Prevalence
- Extensive evidence points to prevalent health problems among the older population. Consider just a few data points:
- Nearly two-thirds of adults over age 65 have gum disease, and one in five has unaddressed tooth decay.1
- Vision loss plagues 37 million Americans 50 years and older. Incidence climbs dramatically after age 60.2 Four serious eye conditions are common among SNF residents: cataracts, glaucoma, diabetic retinopathy, and age-related macular degeneration (AMD).
- Over 58% of moderate to high hearing loss exists among adults above the age of 60 years.3
- 45% of Medicare beneficiaries find it difficult to hear even with a hearing aid.4
- Approximately 20% of adults in middle and old age experience foot and ankle pain. Many of them report debilitating impact on daily activities.5
Care Complications
The challenges of caring for residents’ numerous health issues are exacerbated by several factors. One is that many individuals have significant gaps in their care. For example, about 40% of adults at high risk for vision loss have not seen an eye doctor or received an exam in at least the previous twelve months, while 1 in 11 say they cannot afford the eyeglasses they need.6 Underserved populations are a particular concern. A study of low-income participants in an eye care program showed that 55% had not had an eye examination in 2 or more years, and many screened positive for glaucoma, cataract, diabetic retinopathy, or AMD.7 On the oral care side, a 2021 survey revealed that only half of seniors had seen a dentist in the previous 12 months.8
A second roadblock arises from resident failure to self-report key conditions or relate accurate health information. An extensive study saw that 30% of the adult respondents who were objectively measured to have hearing loss would have remained undetected based on their self-reporting.9 A separate analysis of the same population found that 40% of those with hearing loss did not inform a doctor or nurse.10 Selfreporting gaps stem from multiple factors, including that residents may be asymptomatic for serious conditions at the point of inquiry.
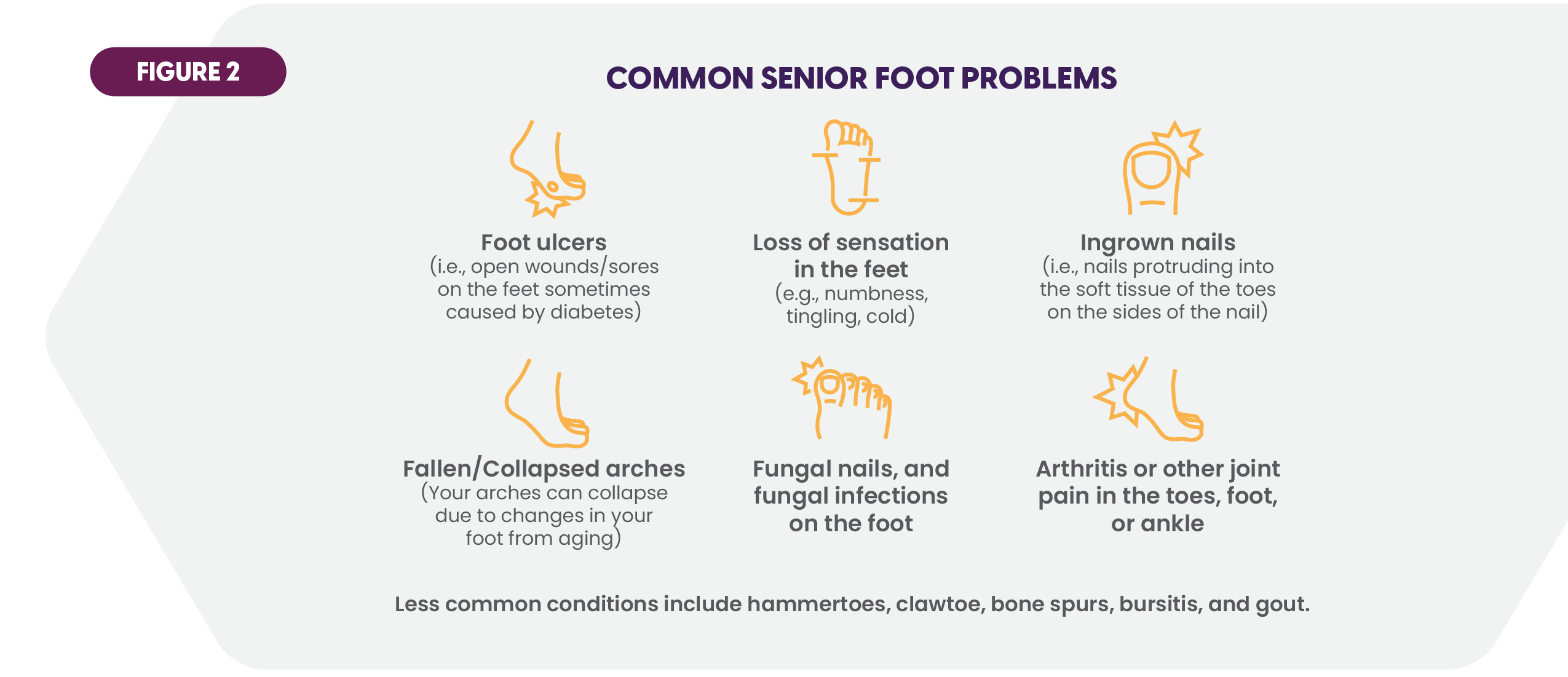
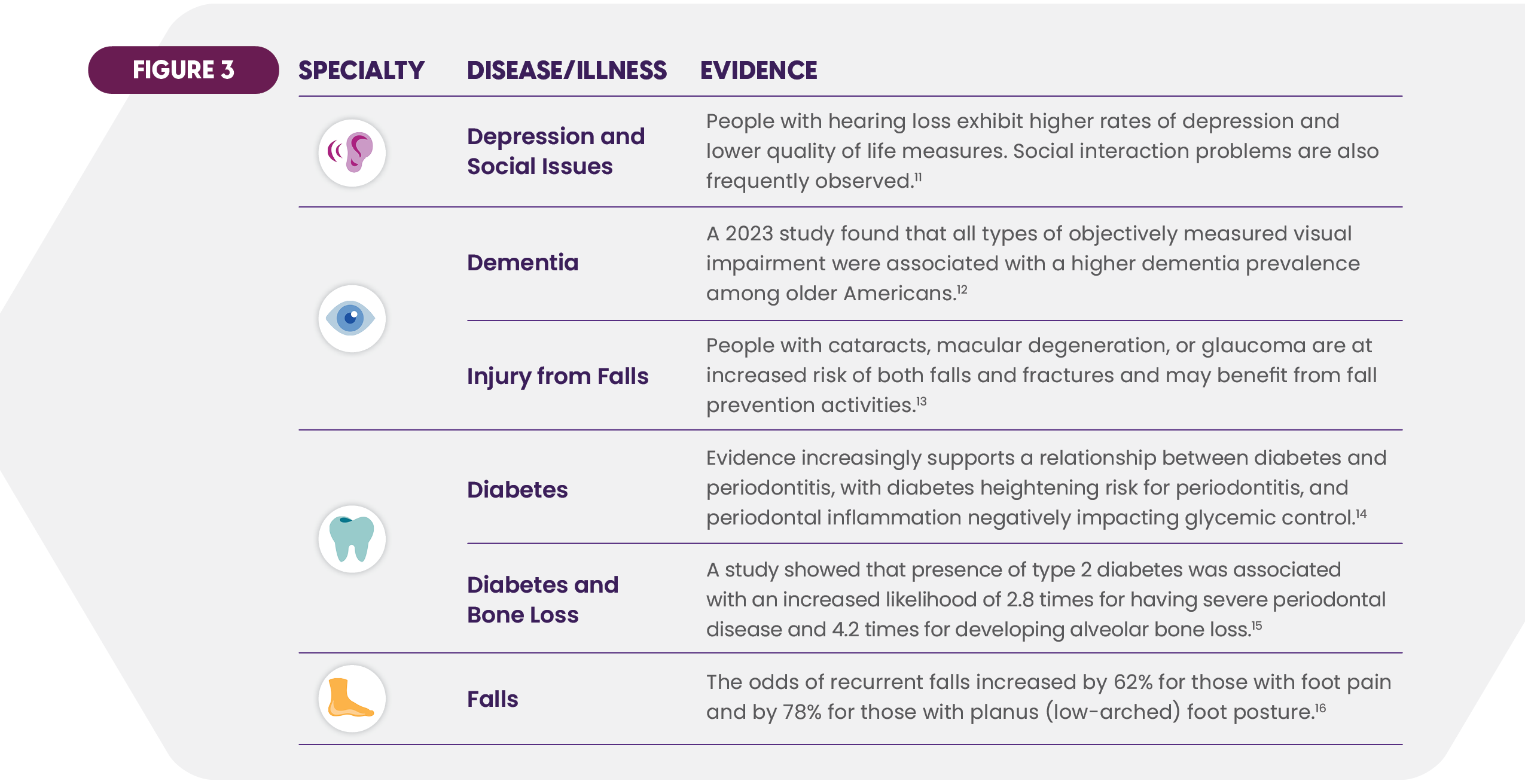
Interactions with Other Diseases
Most SNF residents have comorbidities. Research continues to demonstrate the correlations — often bidirectional — between dental, vision, hearing and foot problems and serious chronic diseases and illnesses. These links jeopardize health, further complicate diagnosis and treatment, and underscore the benefits of vigilant attention to health symptoms.
Drivers of Independent Onsite Ancillary Care
As SNFs juggle numerous clinical and operational priorities, many have turned to external partners to provide onsite ancillary services. Three strong drivers are fueling this trend.
- The magnitude of health problems continues to grow. The aging population portends ever greater demand for healthcare. The number of Americans ages 65 and older is forecasted to reach 82 million by 2050, a 47% increase from 2022 and a rise to 23% of the total population.17 One example of the impact on ancillary services can be seen in the projection that by 2060 moderate to severe hearing loss will increase 157% for those over 80 years old, 38% for those 70-79, and 23% for the 60-69 bracket (figures rounded).18
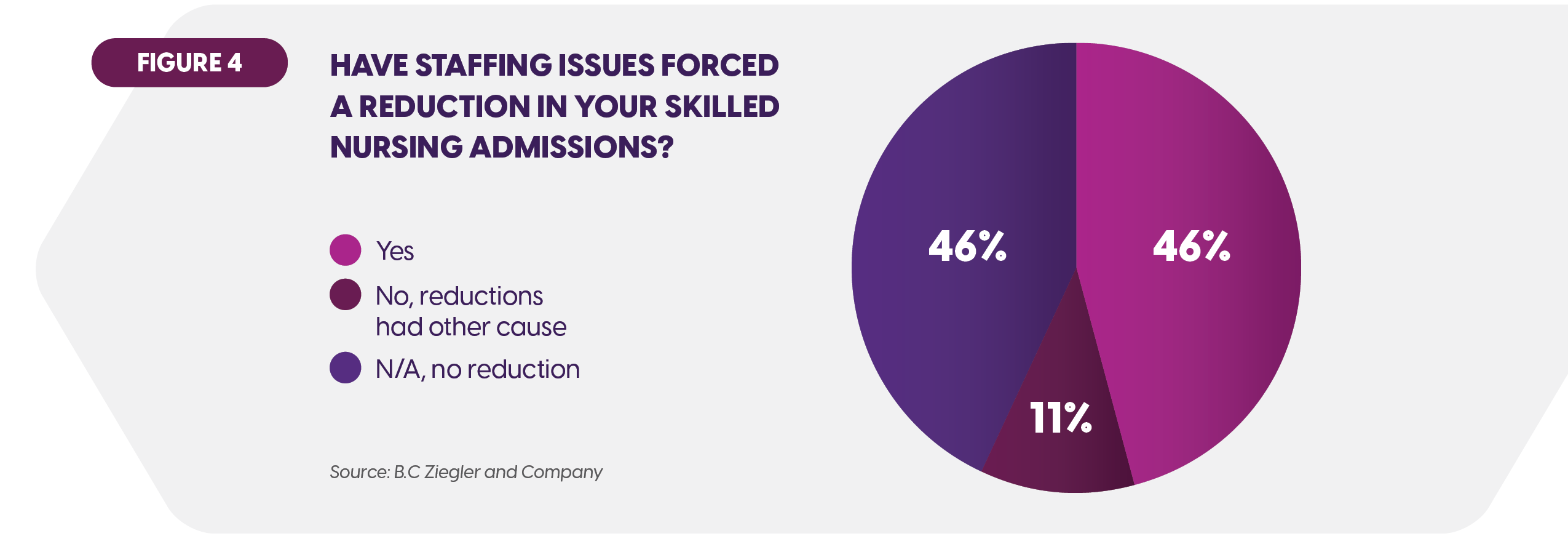
- SNF staffing constraints impede care delivery efforts. Skilled nursing communities are trying to do more with less as workforce shortages persist throughout healthcare, including the post-acute sector. A survey of SNF executives placed “staffing” at the top of their concerns list.19 Forty-six percent of SNFs have experienced declines in admissions attributable to staffing shortfalls.20 This labor environment makes outsourcing an attractive alternative.
- The complex needs in ancillary care call for consistent onsite attention. As this article has detailed, monitoring and treatment of resident dental, vision, hearing, and foot health problems require consistent and thorough onsite care. The growing recognition of that need is further stimulus to engaging external specialists.
Seven Qualities of Compassionate, Comprehensive, Convenient Onsite Care
The providers of ancillary onsite services must demonstrate commitment to care delivery that combines compassion, comprehensiveness, and convenience. Those ingredients are critical to successful outcomes for residents, families, and the skilled nursing communities. Aria’s extensive experience confirms that SNFs should seek the following seven attributes in a partner’s onsite solution.
Care provided to all residents
Onsite ancillary services need to be available across the resident population. External providers must take affordability into account through acceptance of all insurance types as well as offering specialty insurance that may fill needed coverage gaps in private and government plans.
Service range coverage
Bringing residents to various offsite providers can result in episodic care. Performing onsite assessments, regular care reviews, and appropriate treatments helps ensure consistent health monitoring. A comprehensive ancillary services program includes supplying residents with eyeglasses, hearing aids, dentures, and other devices. Full service also stresses both preventive and corrective care. In dentistry, for example, the proportion of adults over age 50 with all of their teeth rose from 14% to 21% in recent years.21 That creates increased need for regular onsite cleanings.
Accommodation of non-mobile residents
Individual care requirements can vary, given that some residents are non-mobile. In such cases, the right provider organization will deliver care in the resident’s room if necessary. The point is to meet residents at their point of need with proactive rather than reactive care.
Understanding of the unique aspects of SNF-based care
Expert ancillary care derives from caregivers with the training and experience to meet health needs common in the skilled nursing environment. The vital competencies include:
- Attentiveness to the mix of resident chronic conditions, comorbidities, and risk factors.
- Knowledge of the relevant regulatory compliance requirements to which SNFs are subject (e.g., F-Tags).
- Strong communication skills to listen well, address concerns and fears, explain care options clearly, and show respect for resident wishes. These strengths must be cultivated. SNFs should also seek external providers adept at communicating with those with memory care issues.
- Ability to build positive relationships with residents to increase willingness to follow the clinician’s care guidance.
The right technology and tools
Effective onsite care requires that clinicians are equipped with the right package of technologies, instruments, and supplies. This “toolkit” should be provided by the partner firm to support disciplined protocols and maintain quality control. Two examples in ancillary care:
Dental:
- Onsite imaging units to capture quality dental images without leaving the facility.
- Portable equipment needed to conduct proper examinations.
- A full set of portable cleaning and prophylactic tools.
- Electronic medical records documentation.
Vision:
- Mobile exam instrumentation and supplies (e.g., autorefractor)
- Appropriate devices to fit, adjust, and repair glasses onsite.
- Comprehensive testing protocol covering visual acuity, eye pressure, side vision, eye movement, cornea, iris, lens, eyelids, retina and optic nerve.
- Electronic medical records documentation.
Collaboration with internal staff
External providers should function as a coordinated extension of the internal care team. SNF staff benefit from advice on resident monitoring while the external clinicians gain alerts and information from the staff that aid the provision of onsite care. This approach is consistent with the consensus that has emerged in healthcare over the past several years which views collaboration among clinicians as the best path to beneficial holistic care.
An integrated medical perspective
Another dimension of care is added when a SNF contracts with a partner for the combination of dental, vision, hearing, and podiatry services. Knowledge-sharing and care coordination among the partner’s clinicians help address the complications that can arise from correlated health conditions in the four disciplines. The SNF care environment becomes more integrated.
Conclusion
The seven qualities outlined offer guidance to SNFs in engaging an onsite provider organization in the increasingly important areas of dental, vision, hearing and foot health. The right partnership furthers the aims of quality care, resident experience, and productive operations. It is a timely solution that deserves consideration by today’s leaders.
Aria Care Partners is the leading provider of onsite ancillary medical services for skilled nursing facilities. With more than 20 years of partnership with over 3,000 skilled nursing facilities, Aria Care Partners remains on the leading edge of innovative care delivery and understanding the connection between dental, vision, hearing, and podiatry services to resident health and well-being. With a unique combination of turnkey insurance solutions and innovative service delivery, Aria Care Partners is passionate about enriching every resident’s quality of life and ensuring that every family knows their loved ones are well cared for and safe.
_____________________________________
 Home Page
Home Page Home Page
Home Page
 Share to Twitter
Share to Twitter
 Share to Linked In
Share to Linked In