Download PDF version here: How Hearing Care Combats Resident Social Isolation and Loneliness
Skilled nursing facilities (SNF) strive daily to maintain resident wellbeing and avoid issues such as isolation and loneliness that frequently afflict older adults. Researchers have established a significant connection between hearing impairment and an individual’s social interaction and mental health. Interventions to counter hearing loss have been shown to be effective in combatting isolation and loneliness.The implications for SNFs are important. Briefly reviewing the evidence sheds light on the high value offered by regular hearing care and use of proven audiology tools to improve hearing capability.
Isolation and Loneliness: A Health Risk Factor
Social isolation has been defined as the “objective state of having few or infrequent social contacts,” and loneliness is “perceived isolation that is distressing for the individual.”1 An estimated 24% of Americans age 65 and older are considered socially isolated, and 43% of adults over 60 report feeling lonely.2
A recent study found that “higher social isolation scores were significantly associated with increased odds of skilled nursing facility stays.”3 Isolation and loneliness pose significant risks to SNF resident overall health. They correlate with a wide variety of negative health conditions. For example, an analysis of multiple studies concluded that low levels of social connection increase the risk of heart disease by 29%, stroke by 32%, premature death by more than 60%, and dementia in older adults by 50%. 4
Hearing Impairment and Social Isolation/Loneliness
Medical research demonstrates that hearing loss and impairment—common among SNF residents—can contribute to a person’s sense of isolation and loneliness. A substantial number of previous studies focusing on these two variables have shown positive correlations with hearing loss.5 Hearing problems make social interaction difficult, leading many individuals to avoid it as a result.
Hearing Interventions: The SNF Onsite Toolkit
Quality hearing care is a vital tool in SNF efforts to minimize resident isolation or loneliness. As a provider of onsite audiology services in SNFs, Aria Care Partners (ACP) sees the benefits of consistent monitoring of hearing health, preventive measures, and timely treatments for specific hearing conditions.
Hearing professionals address hearing loss in several ways. Education about impairment and mitigation options is important in the SNF environment. Audiologists are also able to advise residents, family members, and staff alike on helpful behavioral modifications: speaking more slowly, articulating clearly, understanding issues related to pitch and frequency, conducting face-to-face speech, and many others.
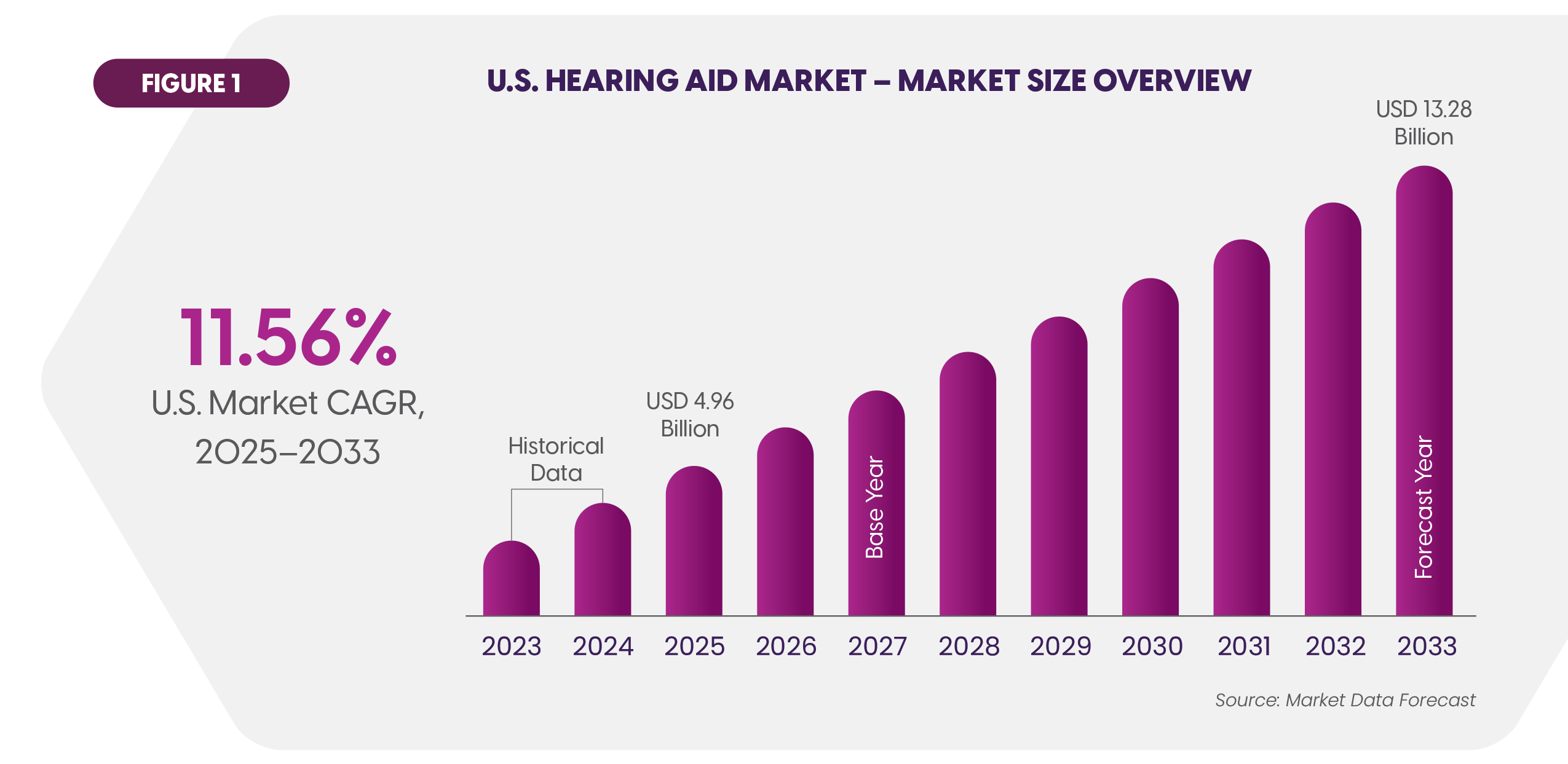
The most prevalent medical intervention is prescription hearing aids. Over 14% of adults aged 65 and higher use aids.6 An estimated 28.8 million American adults could benefit from hearing aids.7 Overall usage is projected to grow rapidly over the next few years (Figure 1).8
Insurance coverage is a significant factor for SNF residents. Basic Medicare does not reimburse for hearing aids. Coverage is available through most Medicare Advantage plans. Medicaid hearing aid coverage is highly variable across the states. Aria Care Partners has long offered plans directly to residents to address their affordability concerns.
Are the Hearing Interventions Effective?
How effective are interventions to improve hearing on reducing loneliness, isolation and adjacent conditions? Investigations over the years have largely confirmed the value of hearing aids as well as cochlear implants that are used in cases of serious hearing loss.
For example, a recent journal article analyzed studies that involved thousands of patients. The authors conclude that “hearing rehabilitation with hearing aids or cochlear implants was generally associated with improved social outcomes, including higher social quality of life (QoL) and decreased perceived social handicap and loneliness.”9 QoL encompasses isolation, loneliness, and social engagement. The positive results indicate that hearing aid use “should be encouraged for those with hearing loss to potentially enhance social engagement.”
Another study with a three year time horizon revealed that participants who received hearing aids achieved beneficial measures for social network diversity, quality, and loneliness relative to a control group.10
Challenges to Overcome
Caregivers confront several common barriers from residents as they seek to take advantage of hearing aids to boost social and mental health:
- Lack of disclosure. An estimated 40% of adults who recognize their hearing loss do not inform their clinicians.11
- Lagging adoption rates. Fewer than a third (29%) of adults aged 71 and higher with hearing loss have used hearing aids.12
- Deferring decisions. According to an extensive study, the average delay by individuals in adopting hearing aids after they become candidates for them is 8.9 years.13
- Perception problems. Cost of hearing aids and a social stigma that some attach to wearing them are common objections. So too is perceived lack of effectiveness caused by issues with fitting or user training.
Experienced audiologists who deliver onsite care can address these issues with residents within the comfort of the SNF setting. They can offer personalized and supportive guidance about the ease of using today’s hearing aids and help ensure proper fit.
Conclusion: The Path Forward
The effectiveness of hearing aids and other interventions on mitigating isolation and loneliness is well supported in the literature as well as in daily clinical observation. This evidence shows how vital a strong onsite hearing care program is to skilled nursing communities’ mission to provide comprehensive care. This care can have meaningful impact on resident social interaction and wellbeing.
References
8 Market Data Forecast, U.S. Hearing Aid Market, June 2025.
 Home Page
Home Page Home Page
Home Page

 Share to Twitter
Share to Twitter
 Share to Linked In
Share to Linked In

