Click to Download a .PDF copy of this article.
Three times around the world is a lot of steps. It’s also a lot of wear and tear on the feet. Nevertheless, it’s the distance the average person walks in a lifetime and helps explain why foot problems are so prevalent among seniors.[1]
Still, common doesn’t mean harmless. In fact, unaddressed foot pain and the underlying causes can have serious ramifications for older adults. Flagging podiatry issues as soon as a resident arrives at a skilled nursing facility can help avert complications, prevent falls, maximize mobility, and support quality of life.
Things to know about aging feet
With 26 bones, 33 joints, 107 ligaments, and 19 muscles, the foot is an amazing anatomical structure and one of the most complex in the human body.[2] For this reason, much can go wrong.
Many foot problems arise simply from aging, as bodily processes slow. Cells don’t regenerate as quickly, affecting the skin. We produce collagen more slowly, which impacts flexibility and the resilience of tissue. Tendons and calf muscles weaken. Protective fat on the bottom of the foot atrophies, leaving bones more vulnerable. Joints stiffen as the amount of synovial fluid that lubricates them decreases. And osteoporosis means new bone production can’t keep up with bone loss.
These age-related changes can affect joints, ligaments, tendons, muscles, and even the ball of the foot. Simple foot problems can quickly spiral, leading to falls, fractures, and/or limb-and-life-threatening infections.
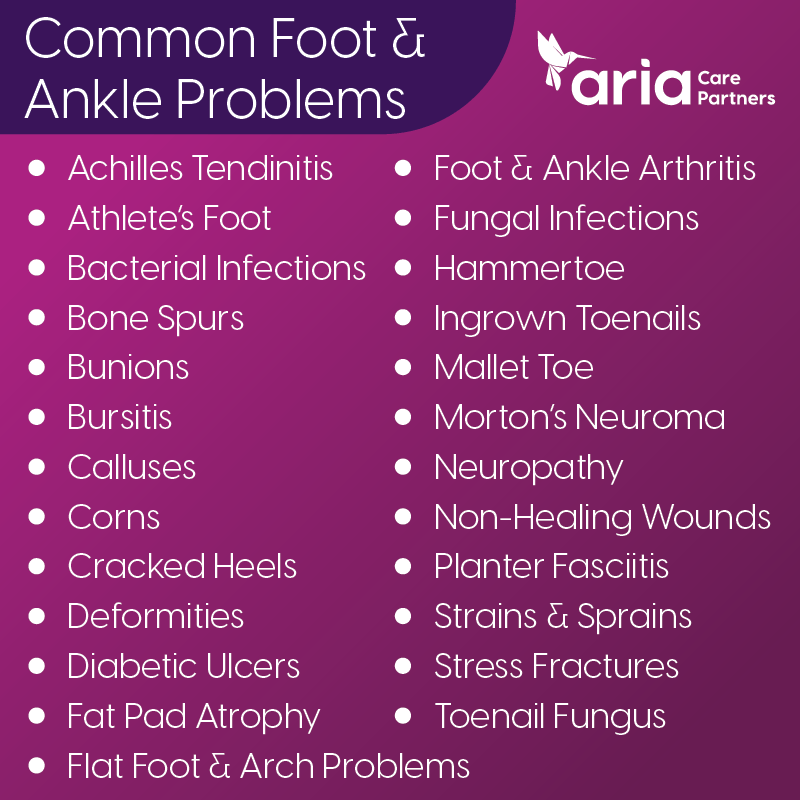
Skilled nursing residents are likely to exhibit one or more of a wide range of prevalent podiatry problems (see image below).
Two special concerns: peripheral artery disease and diabetes
Any foot problem can be a significant matter. Those related to peripheral artery disease (PAD) and diabetes call for heightened attention.
PAD is a cardiovascular disease that develops when blood flow to the arms and legs is diminished due to narrowed arteries, often caused by a buildup of fatty deposits. Typically, it’s part of systemic atherosclerosis. It can lead to non-healing ulcers on the feet and lower legs that rapidly develop complications. Roughly 6.5 million people in the U.S. age 40 and older have PAD.[3]
Nerve damage in the feet of people with diabetes is known as diabetic neuropathy. This condition robs individuals of the ability to feel skin injuries or extreme hot and cold. Consequently, about 5% of those with diabetes develop what’s known as diabetic ulcers on their feet. When these slow-healing wounds are not promptly and adequately addressed, they can escalate to more critical infections and even to gangrene. About 1% of those with diabetes end up with an amputation.[4]
Detecting and addressing any injury to the foot of a resident with PAD and/or diabetes is critically important. Caregivers should contact the resident’s physician immediately.
Ensuring access to expert podiatry care
Given the complexity of the human foot and the extensive range of issues that can arise, it’s important that skilled nursing facilities have easy access to expert podiatry care for their residents.
Maintaining partnerships with experienced, onsite podiatry care providers, like Aria Care Partners, can make it easier for skilled nursing facilities to ensure that all residents get the foot care they need, when they need it. With trained professionals, a consistent disciplined care process, the right equipment onsite, and the ability to accommodate each resident’s on-the-spot situation, Aria Care Partners makes managing podiatry care easier for all and helps facilities comply with wound health regulations.
Teaming with a specialized podiatry care provider that works onsite may be one of the best things skilled nursing facilities can do to protect and enrich the lives of their residents.
Click to Download a .PDF copy of this article.
 Home Page
Home Page Home Page
Home Page

 Share to Twitter
Share to Twitter
 Share to Linked In
Share to Linked In





